Medical assessment and diagnosis
- Introduction
- Medical
Assessment - Medical Assessment
Flowchart - In sport
Time of injury - In sport
Following injury
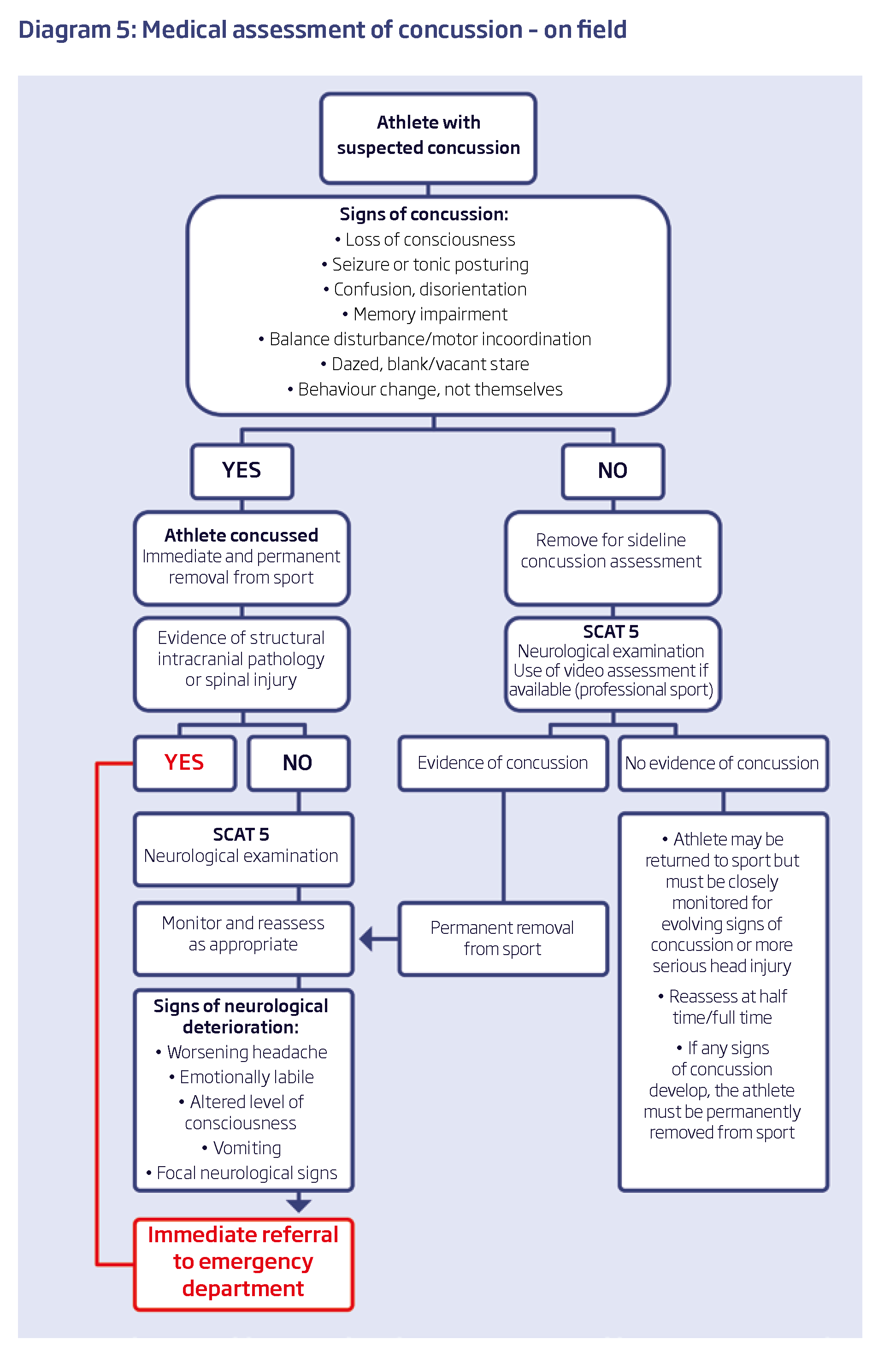
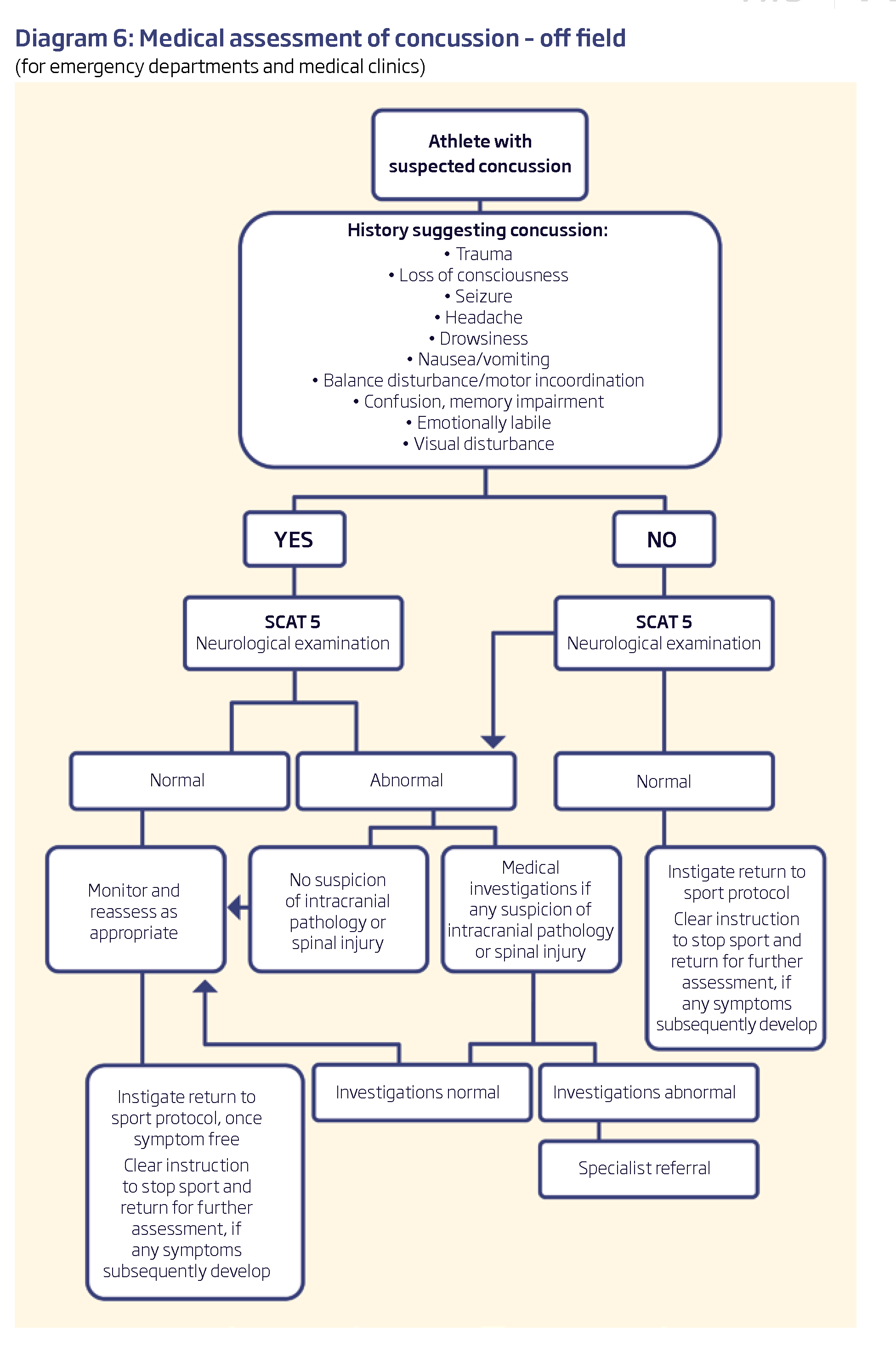
Medical assessment of concussion
Recognising and diagnosing mild TBI is important for treatment and achieving the best outcomes.
The diagnosis of mild TBI should be made by a medical practitioner
The diagnosis should include taking a clinical history and examination that includes a range of domains including mechanism of injury, symptoms and signs, cognitive functioning and neurological assessment including balance testing.
Depending on the nature of the injury CT scans and other assessments may may be required.
The SCAT59,10 is the internationally recommended concussion assessment tool and covers the above-mentioned domains. It should not be used in isolation but as part of the overall clinical assessment. Computerised neurocognitive testing can be undertaken as part of the assessment but again, it should not be used in isolation14. Baseline neurocognitive testing in the pre-season period can be useful for comparison with post-injury scores. Many programs however have reference ranges that can be applied in the absence of a baseline test.
There are currently no serum biomarkers or genetic testing that assist in the diagnosis of concussion15.
Blood tests are not indicated for uncomplicated concussion. Medical imaging is not indicated in the diagnosis or management of uncomplicated concussion15. Medical imaging may be indicated however where there is suspicion of more serious head or brain injury3.
Where resources allow, sporting organisations could use modern technology such as pitch-side instant video replay, to enhance the ability to detect and manage concussion14.
Medical assessment of concussion
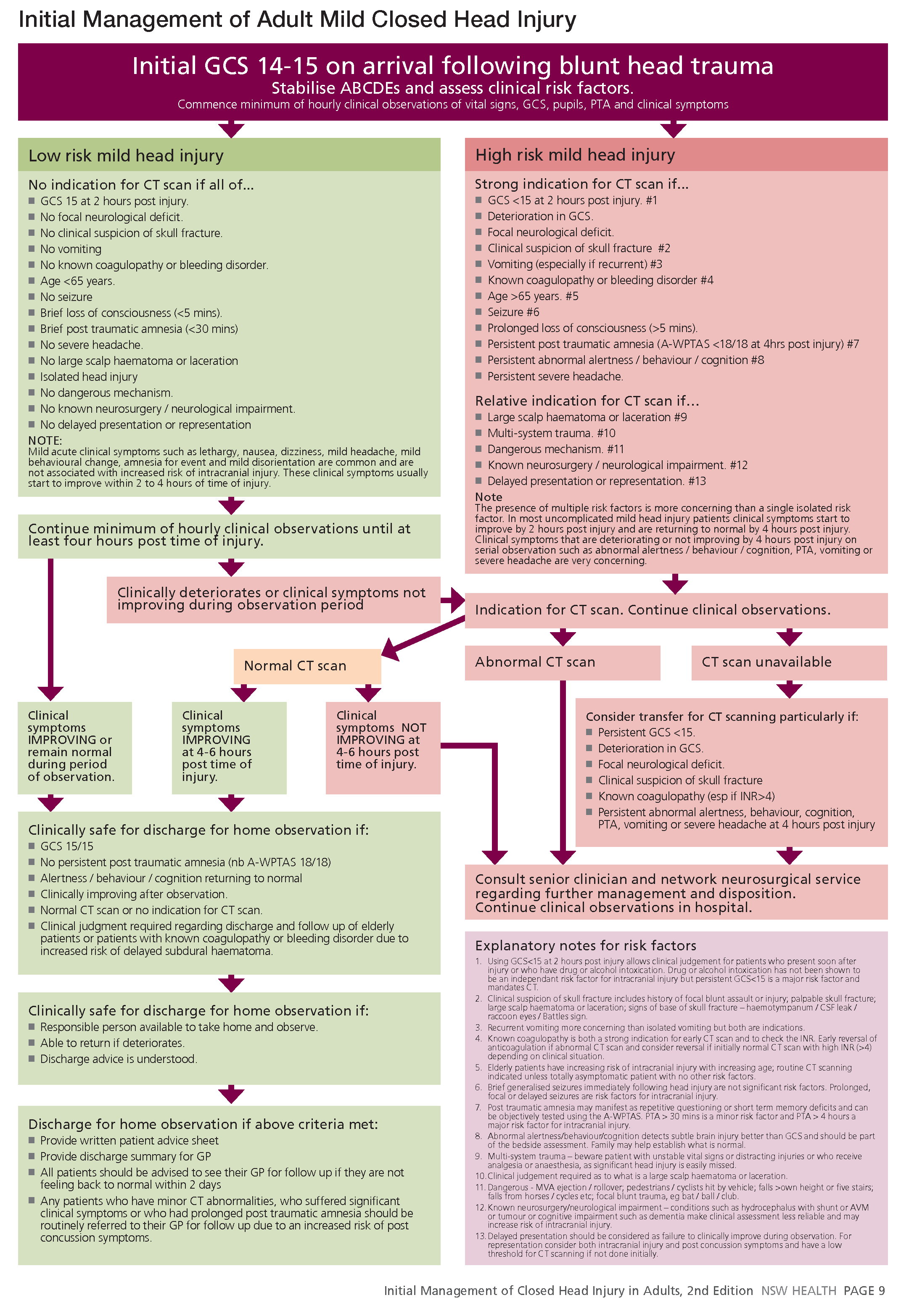
Mild head injury patients should be assessed by a process of structured clinical assessment involving a combination of:
■ initial clinical history and examination
■ serial clinical observations
■ CT scanning if clinically indicated by risk factors identifi ed on initial or serial assessment
Serial clinical observation should include minimum hourly observations of :
■ vital signs.
■ pupillary reactions
■ GCS
■ alertness / behaviour / cognition
■ post traumatic amnesia (PTA) (eg A-WPTAS)
If patients have no signifi cant risk factors for complications of mild head injury and are clinically judged to be “low risk” then they should be observed until at least four hours post time of injury.
If patients have any signifi cant risk factors for complications of mild head injury then they should continue to be clinically observed while further assessment is performed.
Serial clinical observations should be continued on any mild head injury patients who fail to clinically improve at four hours post injury or who are found to have structural lesions on CT scan.
Assessment for PTA should be performed on all mild head injury patients in the emergency department. Mild head injury patients who are admitted to hospital because they have structural lesions, persistent PTA or clinical symptoms should have daily PTA testing until they are shown to be out of PTA.
Clinical assessment using clinical risk factors or clinical decision rules can identify those patients at increased risk of intracranial injury requiring further investigation.
CT scanning is indicated for those mild head injured patients identifi ed by structured clinical assessment as being at increased risk of intracranial injury.
CT scanning is the most appropriate investigation for the exclusion of neurosurgically signifi cant lesions in mild head injured patients
If structured clinical assessment indicates the risk of intracranial injury is low, the routine use of CT scanning is neither clinically benefi cial nor cost effective.
Skull x-rays are not suffi ciently sensitive to be used as a routine screening investigation to identify signifi cant intracranial lesions.